 KMPDC officials said dentists in Kenya face no consequences when they abandon their public duties to earn more in private practice.
KMPDC officials said dentists in Kenya face no consequences when they abandon their public duties to earn more in private practice.Dentists in Kenya appear to have taken moonlighting to
another level. A new analysis from the University of Nairobi reveals that most of those employed in public hospitals routinely skip duties to work in private clinics during official working hours, without facing any repercussions.
The culture is driven by financial need, dysfunctional
public hospitals, and the fact that there are no consequences for stealing work
hours.
The findings, published in Frontiers
in Health Services, note that dentists mostly work in outpatient clinics,
which means they could be absent from work without fatal consequences for
patients.
Dr
Cyril Ogada, a dentist and tutorial fellow at UoN’s department of dental
sciences, conducted the survey in Nairobi alongside Prof
Laetitia Rispel of the University of the Witwatersrand, South Africa.
Their goal was to unearth the state of multiple job holding
among dentists in Kenya. The situation among medical doctors and nurses is
already known.
Multiple
job holding (MJH) refers to working in more than one paid job
concurrently.
“This is one of the first qualitative studies to explore MJH
among dentists in an African and an ambulatory (outpatient) care setting,” they
noted.
Dr Ogada and Prof Laetitia interviewed 30 participants who
included ten dentists and 20 key informants between November 2022 and January
2023.
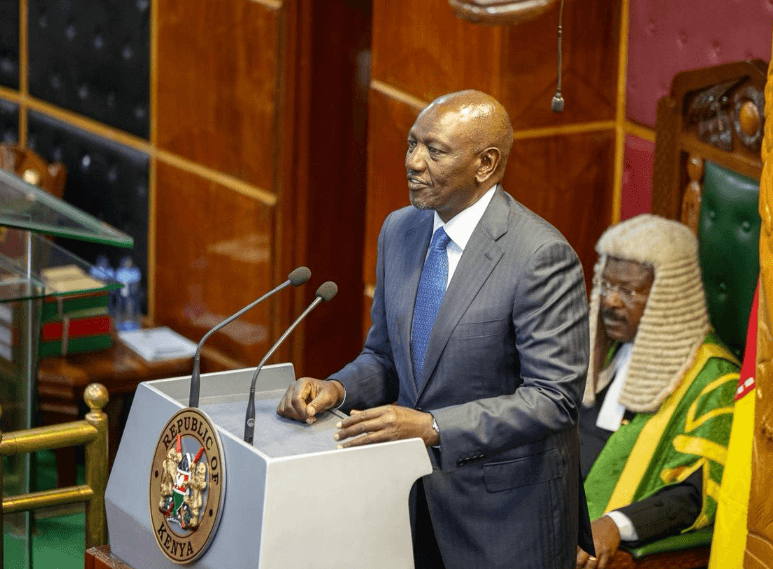
The key informants included officials of the Kenya Medical Practitioners and Dentists Council,
oral health experts, and members of the Kenya
Medical Practitioners, Pharmacists and Dentists Union, and the Kenya Dental Association.
They revealed a troubling culture where stealing entire days
or weeks from a public job to do side hustles is standard practice and is
tolerated.
“Multiple job holding (MJH) is pervasive and has become the
norm, because there are high rewards when dentists engage in MJH, and few or no
adverse consequences due to the unique nature of their work in ambulatory care
settings,” the authors concluded in a paper titled “Dentists are never seen:
perspectives on multiple job holding among dentists in Nairobi, Kenya.”
MJH prevalence among medical doctors in Nairobi is estimated
at 54 per cent, according to a 2021 study. Dr Ogada’s research suggests the
rate among dentists may be just as high, if not higher.
That places Kenya among the countries with the highest rates
of MJH in the world. Only 12.2 per
cent of dental hygienists in the US hold multiple jobs. In South
Africa, it’s 33.7 per cent of doctors and 38.7 per cent of therapists. In
Egypt, 89
per cent of physicians and 73 per cent of dentists moonlight.
KMPDC officials said dentists in Kenya face no consequences
when they abandon their public duties to earn more in private practice.
One official admitted that while public sector contracts
stipulate minimum work hours, “it is the employer who is supposed to know who
is supposed to be on duty at what time”, a responsibility many managers fail to
enforce.
The medics' union, the Kenya Medical Practitioners,
Pharmacists and Dentists Union (KMPDU), also admitted the pervasiveness of this
culture.
“The term that I hear is [that] dentists are just
notorious… [they] just don't come to work,” said one KMPDU official.
“Most young dentists, when they report to their stations, find that it's the culture, and they continue with it.”
The dentists interviewed said money is the biggest
motivator. They said public salaries are fixed and low, especially for
early-career dentists.
“If I were to rely
only on my salary… it is almost impossible to manage many things,” one
respondent said.
Most health workers in the public sector earn a
non-practising allowance to caution them from forgoing income from MJH, the
assumption being that they do not engage in it.
Public-sector dentists in Kenya earn approximately Sh250,000
per month, depending on rank and experience, excluding allowances.
That places them ahead of many clinicians, such as nurses and
clinical officers.
But income is not the only reason. Dentists also said public
clinics are often poorly equipped, and many lack even the basics to do their
work.
MJH gives them not just financial relief, but also access to
modern tools, mentorship, and more complex procedures. These are things they
rarely experience in public hospitals.
“In the public sector, there are many deficiencies in terms
of infrastructure, materials…. If you want to do a root canal, you find you're
still using the old system and the old ways of doing treatment. But in private
practice, there are newer technologies, there is newer equipment, so you're
advancing with the times. So, you're growing,” one of them said.
The study shows that poor patients who rely on public health
facilities pay the cost of MJH. With dentists constantly away at side jobs,
dental clinics in public hospitals open late, close early, or do not operate at
all.
“I remember there's a case we had once at [Hospital X]. A
patient came with a fractured mandible. And they came on a Monday, but the
fracture had happened like two weeks before. So, we asked them what happened.
Why they're coming so late. So, they said they got injured I think on Monday.
Then they were told the dentist doesn't come to work until Thursday. So, they
stayed with that mandible like that until Thursday then the dentist came and
ordered X-rays. And then even after the X-rays were done, you have to wait for
a whole week for the dentist to see you,” one oral health manager recalled.
MJH is not illegal in Kenya. Public Service Commission contracts
require a minimum number of hours per week and offer a non-practising allowance
to dissuade private work. But these measures are not enforced.
Unlike countries like South
Africa, which require prior approval for MJH, or Iran,
which has attempted outright bans, Kenya has no effective system of control or
accountability. Managers rarely confront absentee dentists for fear of losing
them.
“We have fought so hard to get this dentist. If you take him
away, then we don’t have [a dentist],” one hospital manager said.
He said in practice, dentists can steal as many hours as
they want from their government jobs and face no serious risk of sanction.
Lead author Dr Ogada is himself a prosthodontist in Nairobi.
He knows the system from within and wanted to spark discussion about MJH’s
impacts on care quality, professional development, and workforce planning.
“The high reported occurrence of MJH requires a
multi-pronged approach that combines individual, system, and structural
interventions,” he said.
That approach, Ogada and Prof Letitia suggested, should
include better supervision, improvements in equipment and working conditions,
and structured dialogue between unions, employers, and health regulators.










![[PHOTOS] Betty Bayo laid to rest in Kiambu](/_next/image?url=https%3A%2F%2Fcdn.radioafrica.digital%2Fimage%2F2025%2F11%2F3b166e2e-d964-4503-8096-6b954dee1bd0.jpg&w=3840&q=100)


![[PHOTOS]Goons vandalise Nargis Restaurant in Westlands](/_next/image?url=https%3A%2F%2Fcdn.radioafrica.digital%2Fimage%2F2025%2F11%2Fa1c98f6c-2b1d-4b50-b112-1def4d93a193.jpeg&w=3840&q=100)

