Every day, up to nine Kenyan children are diagnosed with cancer. For most
families, the news comes too late, at a stage when treatment is costly,
survival chances are low, and hope fades fast.
Experts warn that unless early detection and access to care improve,
childhood cancer will continue to devastate households and strain an already
burdened health system.
Kenya records more than 3,000 cases of
childhood cancer annually, roughly eight to nine new diagnoses each day.
Yet, the majority of these cases are discovered in advanced stages, when the
disease is harder to treat and survival prospects are minimal.
Doctors say the problem is largely driven by low awareness among the public
and health workers about early warning signs.
Even when cancer is detected early, treatment
remains financially crippling for most families.
Chemotherapy, radiotherapy, and surgery are available locally, but only a
few can afford consistent care.
Many parents resort to selling property, borrowing money, or holding
fundraisers to raise hundreds of thousands of shillings needed for treatment.
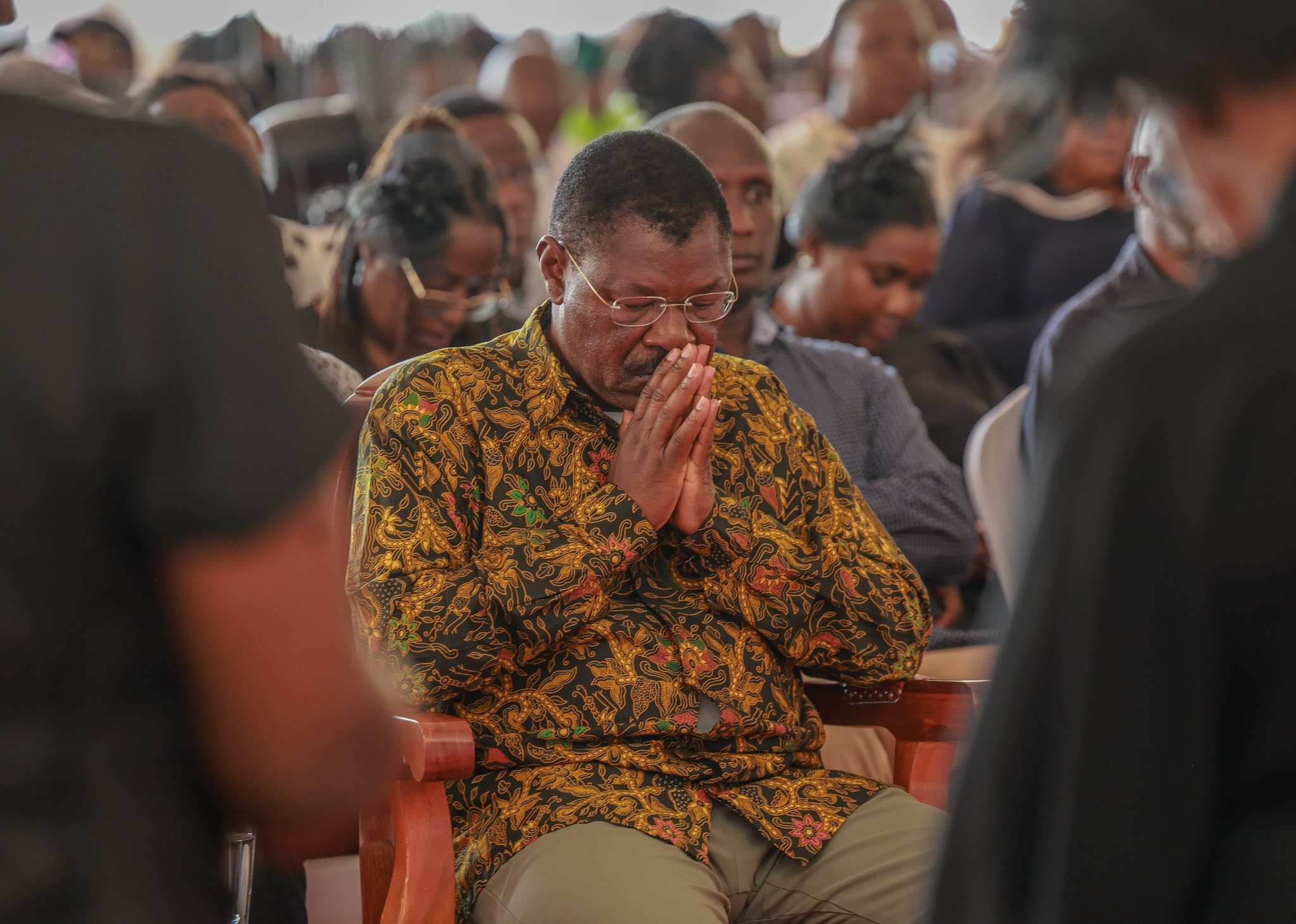
Although the Social Health Authority (SHA) is
designed to cushion families against catastrophic medical costs, coverage for
cancer remains inconsistent.
Most households still pay out of pocket, forcing some children to abandon
treatment halfway or miss vital procedures that could save their lives.
At Kenyatta National Hospital (KNH), the
country’s largest referral facility, the scope of the problem is unmistakable.
Dr. Catherine Muendo, a paediatric haematologist at KNH, says they receive
about 350 new childhood cancer cases every year, a figure that may only
represent a fraction of the real burden.
“In a week, our two paediatric cancer wards
may have up to 80 children. Mondays are the busiest because it’s clinic day,
and we could attend to as many as 70 children,” Dr. Muendo says.
She estimates that Kenya should be diagnosing
around 4,500 childhood cancer cases annually, but only about 3,500 are
reported.
“That means some children are out
there undiagnosed, likely because parents and caregivers are unaware of the
symptoms,” she adds.
For many of those who eventually reach KNH,
the disease is already advanced.
“Parents often tell us they visited several health facilities but were
treated for something else. By the time we diagnose cancer, it has already
spread,” she explains.
Dr. Muendo says the trend points to systemic
gaps: limited awareness, weak diagnostic capacity, and poor referral systems.
“There are no formal screening programmes for childhood cancers. We have to
rely on early warning signs, so awareness among health workers and parents is
critical,” she emphasizes.
Cancer expert and Faraja Cancer Support Trust
CEO, David Makumi, agrees.
He says parents must be alert to subtle but persistent changes in their
children.
“Warning signs include unusual or persistent swelling, easy fatigue,
abdominal lumps, or unexplained bleeding,” he notes.
“It doesn’t necessarily mean a child
has cancer, but it signals that something serious is happening and should be
checked immediately.”
Makumi stresses that parents play a vital role
in early detection.
“Parents need to be the first doctor for their child. If they notice
something unusual, they should raise it with a healthcare provider,” he says.
Some cancers, like retinoblastoma, a cancer of
the eye, can be spotted at home. “You just need to look at the eye. If there is
a glow that wasn’t there before, it needs to be checked immediately,” Makumi
adds.
He warns that childhood cancer is becoming a
major public health problem that demands urgent action.
“If we want to improve survival, we
must make cancer medicines for children available all the time. We also need the
Social Health Authority to cover everything so parents don’t have to go back to
their pockets to pay,” he says.
Globally, the World Health Organization (WHO)
estimates that about 400,000 children and adolescents aged 0–19 are diagnosed
with cancer each year.
The most common types include leukemia, brain tumours, lymphomas, and solid
tumours such as neuroblastoma and Wilms tumour.
Survival rates vary sharply depending on location: more than 80% of children
in high-income countries are cured, while fewer than 30% survive in many low-
and middle-income nations.
The difference is largely due to late diagnosis, lack of access to essential
medicines, and weak health systems.
Unlike adult cancers, most childhood cancers
do not have identifiable causes.
They are rarely linked to lifestyle or environmental factors. Instead, they
result from genetic changes in growing cells.
Some infections, including HIV, Epstein-Barr virus, and malaria, may
increase risk, while vaccinations such as hepatitis B and HPV can prevent
cancers that develop later in life.
Experts emphasize that early diagnosis is the
cornerstone of improving survival. WHO outlines three essential steps:
awareness of symptoms by families and primary care providers, accurate and
timely clinical evaluation, and prompt access to treatment. When detected
early, children respond better to therapy, need less aggressive interventions,
and experience fewer complications.
In Kenya, however, many frontline health
workers lack specialized training to recognize the early signs of cancer in
children.
Symptoms are often mistaken for common illnesses like malaria or bacterial
infections, delaying proper treatment.
Geographical and economic inequalities also
compound the problem. Children in rural counties face delays in referrals
because local health facilities lack diagnostic tools or trained specialists.
Many families travel long distances
to national referral hospitals in Nairobi or Eldoret, incurring additional
transport and accommodation costs.
Makumi says this underscores the need to
strengthen regional cancer centres.
“We must decentralize services so that families outside major cities can
access timely diagnosis and treatment. That’s the only way to improve survival
rates,” he explains.
Treatment for childhood cancer typically
combines chemotherapy, surgery, and radiotherapy.
When delivered effectively, cure rates can exceed 80%.
Many required medicines are inexpensive generics included in WHO’s essential
medicines list for children. Still, care must go beyond medical treatment.
Children need proper nutrition, psychosocial support, and continuous
monitoring of their growth and development. Survivors also require long-term
follow-up to detect relapses and manage possible side effects.
For those who cannot be cured, palliative care
offers relief from pain and helps maintain quality of life.
Experts say such support should begin
at diagnosis and continue throughout treatment.
However, access to palliative services and essential pain medications such
as oral morphine remains limited in many parts of the country.
The fight against childhood cancer demands
collective effort — from government, civil society, and communities.
Kenya’s participation in WHO’s Global Initiative for Childhood Cancer, which
aims to achieve a 60% survival rate worldwide by 2030, offers hope. But on the
ground, success will depend on timely diagnosis, affordable treatment, and a
steady supply of essential medicines.
As Dr. Muendo and Makumi both emphasize, Kenya
has the capacity to turn the tide.
“If medicines are available, if
parents are alert, and if healthcare workers act fast, we can save many more
children’s lives,” Makumi says.