The Ministry of Health has launched a crackdown on fraud in Kenya’s healthcare sector, warning hospitals, doctors, and patients that perpetrators will face the full force of the law.
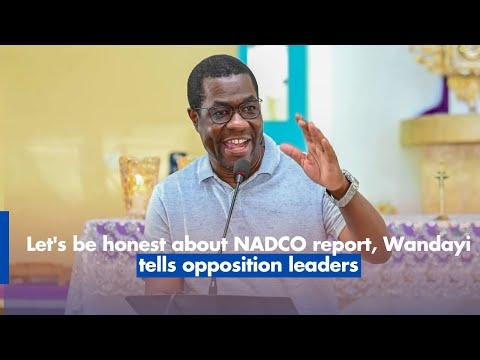
In a press briefing at Afya House, CS Aden Duale said the campaign is a cornerstone of the Taifa Care programme, describing it as an “uncompromising stance against fraud” and a constitutional obligation.
Duale disclosed that fraudulent claims are draining billions from the Social Health Insurance Fund (SHIF).
Out of Sh82.7 billion in claims submitted, Sh10.6 billion has been rejected due to fraud or non-compliance, while another Sh2.1 billion remains under surveillance.
“Our position on safeguarding public resources has been consistent, clear, and unwavering. The concerns now being raised are not new; they have been an integral part of our public discourse and enforcement actions from the very beginning,” he said.
"This position is rooted in our constitutional obligation under Article 43(1)(a) of the Constitution of Kenya, which guarantees every Kenyan the right to the highest attainable standard of health. To fulfil this right, we must ensure the prudent and accountable use of public funds, as mandated by the Public Finance Management Act. Every shilling contributed to the Social Health Insurance Fund must go towards legitimate, life-saving healthcare.”
Duale said that since assuming office on April 1, 2025, he has intensified the fight using a digital system designed to flag anomalies.
He noted that the system is becoming more effective with time, and the more data the system collects, the easier the detection of fraud becomes.
The CS said that audits have already uncovered serious malpractice, including up-coding, falsification of records, and phantom billing in health facilities across the country.
Duale said the ministry will not tolerate such practices and that any facility, doctor, or patient found to be involved in fraudulent activities will be held liable and face the full force of the law.
He said the government is also moving to recover funds already lost and will engage law enforcement agencies in the process.
On the issue of NHIF legacy debt, Duale assured Kenyans that all verified claims worth between Sh0 and Sh10 million will be paid.
However, larger claims will be subjected to thorough verification before settlement.
He further clarified that the Social Health Authority’s contracts are strictly with individual facilities, not associations.
As part of the broader crackdown, the ministry has entered into a new partnership with top medical insurers to establish a Joint Anti-Fraud Action aimed at tightening oversight and accountability.
“Our work has just begun. We will not rest until every Kenyan has access to quality, affordable, and dignified healthcare, free from the burden of fraud.”