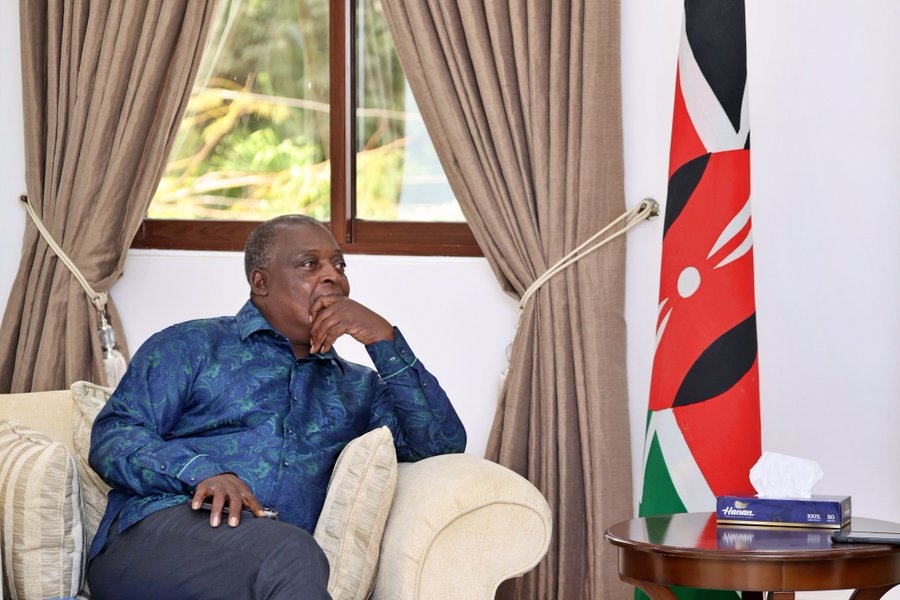
Health CS Aden Duale delivers a comprehensive update on the rollout of Taifa Care on June 16, 2025/HANDOUT
Health CS Aden Duale delivers a comprehensive update on the rollout of Taifa Care on June 16, 2025/HANDOUT
Kenya’s push toward Universal Health Coverage (UHC) is gathering momentum under the Taifa Care programme.
Millions are already benefiting from reforms that are transforming the country’s healthcare landscape.
Speaking at Afya House on Monday, June 16, Health Cabinet Secretary Aden Duale described the changes as “a people-centered revolution” aimed at making healthcare more affordable, accessible, and accountable.
“We are not just expanding access—we’re cleaning up the system,” Duale said.
Since the rollout of Taifa Care in October 2024, more than 23.6 million Kenyans have enrolled with the Social Health Authority (SHA), the government body implementing the Social Health Insurance Act of 2023.
Of these, 5.7 million have already accessed services at public, private, and faith-based health facilities.
According to CS Duale, more than 3.6 million received free treatment for common illnesses, while 2.1 million benefited from specialised care, including 400,000 dialysis sessions and 17,000 cancer treatments.
Alongside increased access, the government is cracking down on fraud and unlicensed health providers.
In partnership with regulators, the Ministry has closed 728 non-compliant health facilities and downgraded 301 others. Duale warned that SHA-contracted facilities must meet strict standards.
To support this effort, a digital tracking system has been introduced to monitor patient visits and prescriptions in real time, helping eliminate fake drugs and inefficiencies across the health sector.
The government is also making major investments in healthcare workers and infrastructure.
The 2025/26 budget allocated Sh6.2 billion to hire UHC contract health workers, Sh1.75 billion to clear pending medical bills, Sh4.2 billion for onboarding intern doctors, pharmacists, and clinical officers, and Sh3.2 billion for training and supporting community health promoters.
An additional Sh13 billion is earmarked for primary healthcare and Sh8 billion for managing emergency and chronic illnesses.
For informal sector workers, the government has rolled out the Lipa SHA Pole Pole plan—an interest-free, flexible payment option based on income levels.
So far, 1.8 million contributors have signed up, already surpassing NHIF’s best annual record.
“No longer will a mama mboga pay the same as a CEO,” said Duale.
“We’ve replaced the flat-rate system with fairness.”
The Social Health Authority has also introduced reforms to speed up payments to hospitals. Facilities are now reimbursed by the 14th of every month.
Since October 2024, Sh43.8 billion has been paid out, including Sh6.2 billion just last week.
To keep essential drugs and medical supplies available, KEMSA has been recapitalised and a Sh10 billion revolving credit facility established.
In an effort to lower the cost of specialised care, the Ministry is partnering with leading private hospitals like Aga Khan University Hospital and The Nairobi Hospital.
Services such as cancer and kidney treatment will be available at government-subsidised rates with no out-of-pocket expenses.
A separate partnership with Roche Pharmaceuticals has reduced the price of breast cancer drug Herceptin from Sh120,000 to Sh40,000, significantly easing the financial burden for patients.
The next phase of digitisation will expand to seven additional counties, including Kisumu, Wajir, Machakos, and Nakuru.
Plans are also in place to roll out a public-facing service charter and step up SHA registration in underserved regions.
“We are accelerating reforms, rooting out ghost facilities and quack doctors, and investing in a future where health is a right, not a privilege,” Duale said.
He also called on union leaders to embrace dialogue, assuring health workers that the government is acting in good faith.
“This is a government that acts—not just talks," CS Duale said.