Despite multiple challenges, counties across Kenya are developing innovative strategies to strengthen health emergency response systems and prevent avoidable health crises.
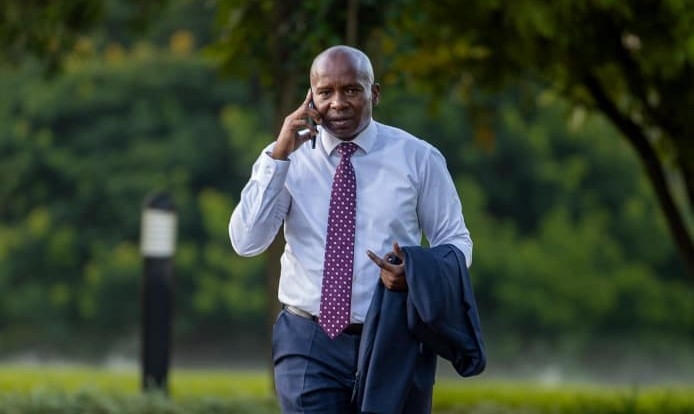
Dr Benjamin Wachira, Executive Director of the Emergency Medicine Care Foundation (EMKF), notes that while progress has been made, significant gaps remain.
Counties are actively working to address these gaps to ensure timely emergency care — a move that could reduce preventable deaths by up to 50 per cent, according to World Health Organisation (WHO) estimates.
A major challenge, he explains, is inadequate infrastructure and limited ambulance coverage, particularly in remote and hard-to-reach regions. In Marsabit County, for instance, vast distances and poor road networks make emergency response difficult.
The County Executive Committee (CEC) Member for Health, Malich Boru, says the county faces shortages of ambulances and logistical challenges due to difficult terrain.
Even so, he notes, Marsabit has invested in additional ambulances and referral coordinators. However, persistent challenges such as limited funding, inadequate equipment, and poor network coverage continue to hinder progress.
The end of donor support has also strained outreach and mobile clinic services that serve isolated communities.
In Kilifi County, emergency health systems have evolved significantly. Previously uncoordinated ambulance operations have been centralised, improving dispatch efficiency and response times.
The county has also set up an emergency medical services unit staffed by trained personnel, enhancing integration between pre-hospital and hospital care.
Kilifi has additionally launched first aid training for community health promoters and local first responders, including boda boda riders, to enable immediate care before ambulances arrive in remote areas.
Dr Wachira emphasises the importance of structured plans and national coordination to expand such initiatives. He notes that more than 10 counties now have organised emergency health systems, including public ambulance services with centralised communication, emergency departments, and trained staff.
“The national government’s efforts — through Kenya’s Emergency Medical Care Policy 2020–2030 and the establishment of dedicated emergency funds — are helping counties build sustainable systems,” says Dr Wachira.
He adds that because emergencies occur in communities, not hospitals, the response must begin immediately through trained local responders and efficient ambulance services connected to well-equipped emergency centers.
While acknowledging that establishing fully functional emergency systems takes time, Dr Wachira highlights the steady progress made in the past decade — from virtually no services to growing county-level capacity.
“We need to sustain the current momentum so that at least half of all counties have well-coordinated emergency services by 2027, and aim for universal coverage by 2030,” he says.
He further stresses that partnerships between counties and organisations such as EMKF and USAID are vital for expanding capacity, training, and infrastructure.
Through ongoing investments in training, infrastructure, ambulance fleets, communication systems, and community involvement, counties are steadily improving emergency response capabilities — ultimately saving more lives.
“Emergency care must find the patient, stabilise them, and transport them to the hospital,” Dr Wachira concludes.
“If implemented effectively across all counties, this approach can reduce preventable deaths by up to 50 per cent.”