The government is preparing for another round of medical equipment scheme because health facilities are unprepared for Universal Health Coverage.
The intended upgrade will target low level facilities such as dispensaries by equipping them with basic equipment.
Most services in the relaunched UHC should be offered in dispensaries, health centres and level four facilities.
However, the Kenya Health Facility Census 2023, released last month, shows only seven per cent of health facilities in Kenya are ready to offer basic outpatient services.
Preparedness means a facility should have all the requisite infrastructure, staff and equipment.
These equipment include basic instruments such as thermometer, weighing scales, stethoscope, blood pressure machine, pulse oximeter, drip stand, oxygen cylinder, stadiometer and examination couches, among others.
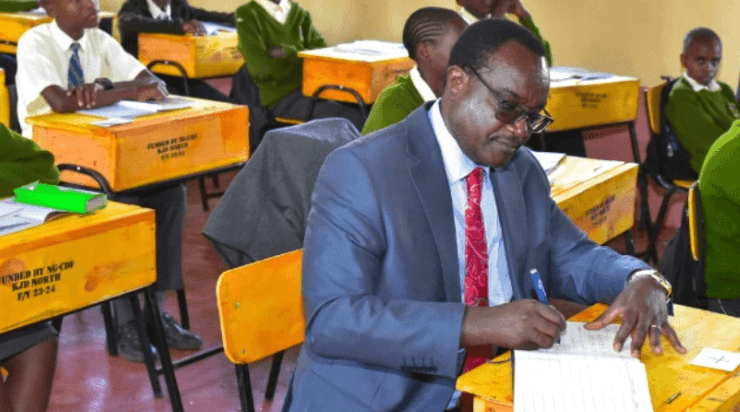
“Availability of basic equipment is especially a critical gap that needs to be bridged for quick gains,” acting Director General for Health Patrick Amoth said.
The survey targeted 14,366 health facilities including public (47 per cent), private (46 per cent), faith-based/non-governmental organisations health facilities (eight per cent).
It shows although more than 80 per cent of health facilities have a reliable power and water source, half (51 per cent) lack access to functional ambulances.
“Investments should be made to increase facilities connected to piped water from 45 per cent and ensure all weather access to all facilities,” the report said.
Health Cabinet Secretary Susan Nakhumicha said the Facility Census 2023 aimed at providing baseline information on service availability, readiness of health facilities to deliver services, availability of human resources and health infrastructure across all health facilities and in turn provide a framework to inform investments to address critical gaps in health service availability and readiness.
She said determining the level of availability and readiness of health facilities to offer services, as well as the quality of care across the sector, is paramount in planning for UHC implementation.
“The data will support health sector reviews and evidence-based decision-making for strengthening country health services,” she said at the launch of the report.
Nakhumicha said the findings will be instrumental in informing planning, policy formulation and programming within the health sector.
“The identified gaps and inefficiencies shall also guide investments within the sector to ensure optimal delivery of quality health care and accelerate the attainment of Universal Health Coverage in Kenya,” she said.
The government is banking on the proposed, highly controversial 2.7 per cent gross income tax to fund its UHC plan.
The tax is projected to raise at least Sh500 billion every year.
According to the ministry, once the UHC is rolled out, Kenyans should access free specialised care in health facilities.
However, less than half of the facilities in the country offer maternity services with only a third of the facilities offering emergency obstetric care, according to the report.
Despite a majority of the facilities having adequate delivery beds and delivery packs, critical gaps were noted such as; only 40 per cent of the facilities offered blood transfusion services while only 54 per cent of the facilities had a source of oxygen.
“Investments are critically needed in equipment, supplies and human resource to deliver both basic and comprehensive maternity services and for newborn care (vacuum extractors, resustiares, Oxygen source, among others). This impacts negatively on maternal and newborn health outcomes and is a barrier to improving quality of care during and after delivery,” the report says.
Several studies show if properly implemented, a UHC plan has huge returns.
One recent study suggests that for every shilling that Kenya invests in primary healthcare, it will save Sh16 treating certain diseases in the future.
Researchers said a well-resourced basic health system will not only lead to substantial health benefits, but also spur economic growth.
They discouraged huge allocations to chronic diseases, at the expense of basic services at the village dispensary.
Some of the researchers are affiliated with the Ministry of Health, others with the University of Nairobi, Unicef and policy think tank Futures Health Economics and Metrics Limited.
Their findings support the relaunched UHC, which is heavy on basic health services.
In the current set up, the government is hiring a 100,000-strong team of community health workers to support the UHC.
The researchers conducted a cost-benefit analysis of running such a system.
“Every $1 [Sh157] invested in PHC interventions saves up to $16 [Sh2,522] in spending on conditions like stunting, non-communicable diseases, anaemia, tuberculosis, malaria and maternal and child health morbidity,” they said.
Their findings, titled Investment case for primary healthcare in low- and middle-income countries: A case study of Kenya, are published in the Plos One journal.
Primary healthcare refers to the most basic package of essential health services and products needed to prevent disease, promote health and manage illness.
According to the World Health Organization, it typically covers about 80 per cent of a person’s health needs during their lifetime.
Most of these services are offered in the community and through dispensaries and health centres.
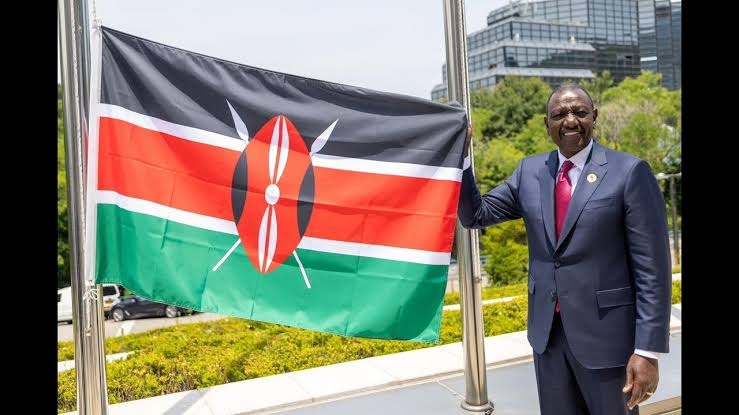
While relaunching the UHC in October, President Ruto said there will be no direct co-payment for services in all the level 1, 2 and 3 facilities.