When every member of the United Nations signed on to the Astana Declaration in October 2018, it offered a new commitment to making comprehensive primary care available and accessible to all.
Every visible commitment by national governments, development partners, and professions was heartening and hopeful.
The COVID-19 pandemic exposed inequities in health care across the globe, specifically in terms of access to appropriate testing, treatment and essential vaccinations when they became available.
In fact, it has brought us to the realisation that not every illness or disease requires hospital treatment.
More than 80 percent of routine illnesses, diseases, and chronic conditions can be more appropriately managed in a community setting with the support of a medical practitioner and primary care team.
Addressing health inequities has to be the biggest challenge we face if we are to achieve the promise of our nations for universal health coverage.
It requires resource commitments of money and people to train the professionals who make up the primary care teams.
It also requires foresight and planning to assess and anticipate the numbers of each professional group needed to serve the population.
Furthermore, it needs political leadership to follow through on a longer-term goal when political goals tend to be short-term and election-led.
In countries that continue to need financial and technical support for their health systems, it needs the commitment of the development partners "to put their money where their mouth is” and preferentially support the establishment and expansion of programs that will deliver comprehensive primary care.
To achieve universal health coverage, we need to be working together, across nations and regions, to ensure that the cadres of professionals who make up primary care teams are being recruited, trained, and offered professional development.
This is because they can provide the range of primary care services necessary to ensure that population groups have their health needs addressed appropriately and remain productive.
As we come through the worst of the effects of the pandemic, we need to revise our view of our health systems.
A health system based on accessibility to comprehensive primary care (rather than secondary care) delivers the best outcomes, at a lower cost, and builds long-term trust between a primary care team and their patients.
Of course, secondary care services will be needed, but they are to support patients who cannot be supported in the primary care system.
Strengthening the primary care system will reduce the inappropriate demand for secondary care services, by addressing most health needs earlier and more appropriately.
As medical practitioners write around the world, they need to get that message across loud and clear and at every possible opportunity.
They must use their collective and individual voices to persuade, convince, influence, and show the way.
Medical practitioners know the components of a good primary care strategy.
They understand how different professional cadres can work together to achieve the best health outcomes in a community.
They know the complexities of providing health care to people from "the cradle to the grave" and all the major life events in between.
Their knowledge of the patients they handle and the trust the patients have in them is developed over a lifetime.
Piecemeal development will not achieve the goal, especially when it is not supported by the professional development of primary care team members.
We need a quantum shift in emphasis towards creating a platform for delivering comprehensive primary care for everyone.
As in many other facets of life, most medical practitioners adopted technical changes during the pandemic.
While these changes facilitated communication, they could never replace face-to-face contact.
Delivery of primary care had to adapt and change to suit the prevailing need for caution and protection, both for patients and health professionals.
Virtual consultations cannot and will never completely replace face-to-face consultations.
But there are occasions and circumstances when a virtual consultation is exactly what is needed or what is most appropriate.
We need to be open to the opportunities presented by new means of delivering care directly to patients and embrace those opportunities where they make the achievement of universal health coverage a reality.
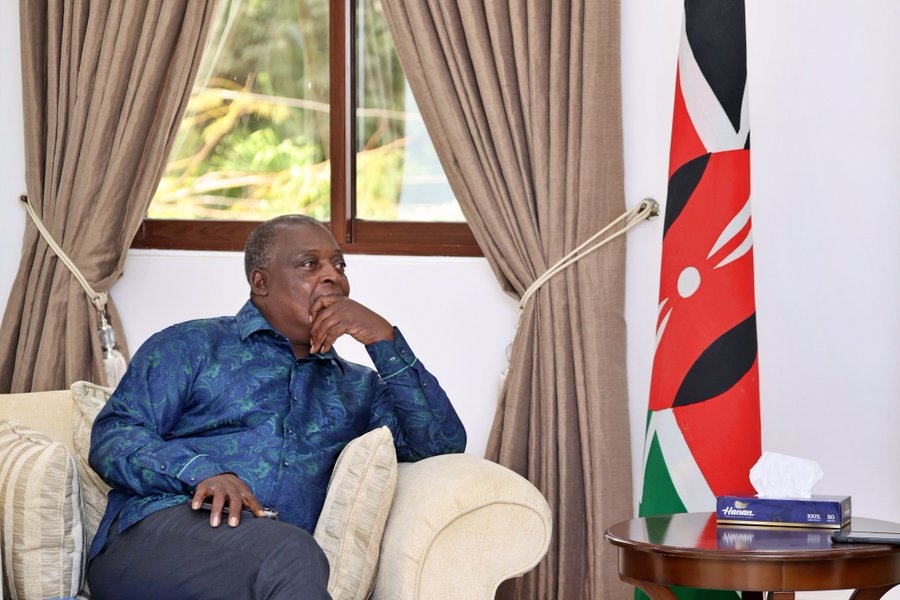
The evidence of the Kenyan Government's efforts to realize Universal Health Coverage as espoused in the Kenya Kwanza Manifesto supports the premise; implementation is now key.
Dr. Humphrey Young, PhD is Public Policy & Development Expert