At Lodwar Teaching and Referral Hospital, patients, mostly women and their children, wrapped in colorful beads, wait patiently in line at the outpatient wing.
Their eyes carry stories of endurance. Their dusty rubber sandals tell of long walks in this county’s vast land in search of health, a good number for a condition they can neither pronounce nor know the origin.
Beyond the hopeful chatter, the atmosphere shifts. Inside the inpatient wards, the air is thick with antiseptic and the weight of suffering.
Beds providing temporary comfort for these patients with distended bellies overflow into the corridors, leaving little room for dignity or rest.
Flies drift through the heat, weaving between the joyful laughter of those being discharged.
Some have recovered from broken bones, others the nurses discharge and they smile as they pack and prepare to go home, and a mother holding a newborn baby after a safe delivery.
However, not all are lucky, as a few are left behind. Soft, pained moans of those still fighting for their lives with noses bleeding or swollen limbs and yellowed eyes with no appetite rent the air.
On thin mattresses, bodies lie curled and fading, caught in the grip of this ancient and merciless neglected tropical disease or Kala-azar, as most Kenyans know it.
In these Kala-azar corridors, a grandmother with a big smile tends to a frail boy, perhaps her grandson.

A man paces nearby, feeding his relative a slice of watermelon, the only food he can afford.
Inside the ward, in a far corner, Philip Ewoi lies motionless. His skin is jaundiced, his limbs swollen. His teary wife, hands trembling, wipes his forehead with a damp cloth.
“He was strong,” she murmurs. “Now, even lifting his hand is too much.”
Philip struggles to sit up and greet the visitors. Philip is suffering from Kala-azar.
Turkana county, located in the northern part of the country, is a land of extremes, well known for beautiful sandy beaches, a great annual cultural festival, minerals, oil and irrigation schemes.But on the other extreme, hunger, scorching sun, vast distances, and sudden floods that leave behind mud where sand flies breed.
One in every 5 children is currently suffering from global acute malnutrition, with the food insecurity situation currently classified as an emergency in many parts of the county.
Villagers and herders sleep outside near anthills, unaware that the tiny insects biting them in the early morning may carry a death sentence.
Young boys who herd goats sleep outside in cool places near anthills, returning home with fevers that do not break.
Many people seek alternative treatments, delaying contact with the formal health systems.
Unfortunately, by the time they reach treatment centres they are suffering from malnutrition with extremely low blood levels that often leads to dire outcomes.
By the time they reach a hospital, many are beyond saving.
Kala-azar is a parasitic disease transmitted by sandflies. It devours its victims slowly, draining blood, swelling organs, and hollowing faces.
Despite the availability of lifesaving drugs through philanthropy, treatment often needs to be supplemented by blood transfusions and nutrition supplements which are often unavailable.
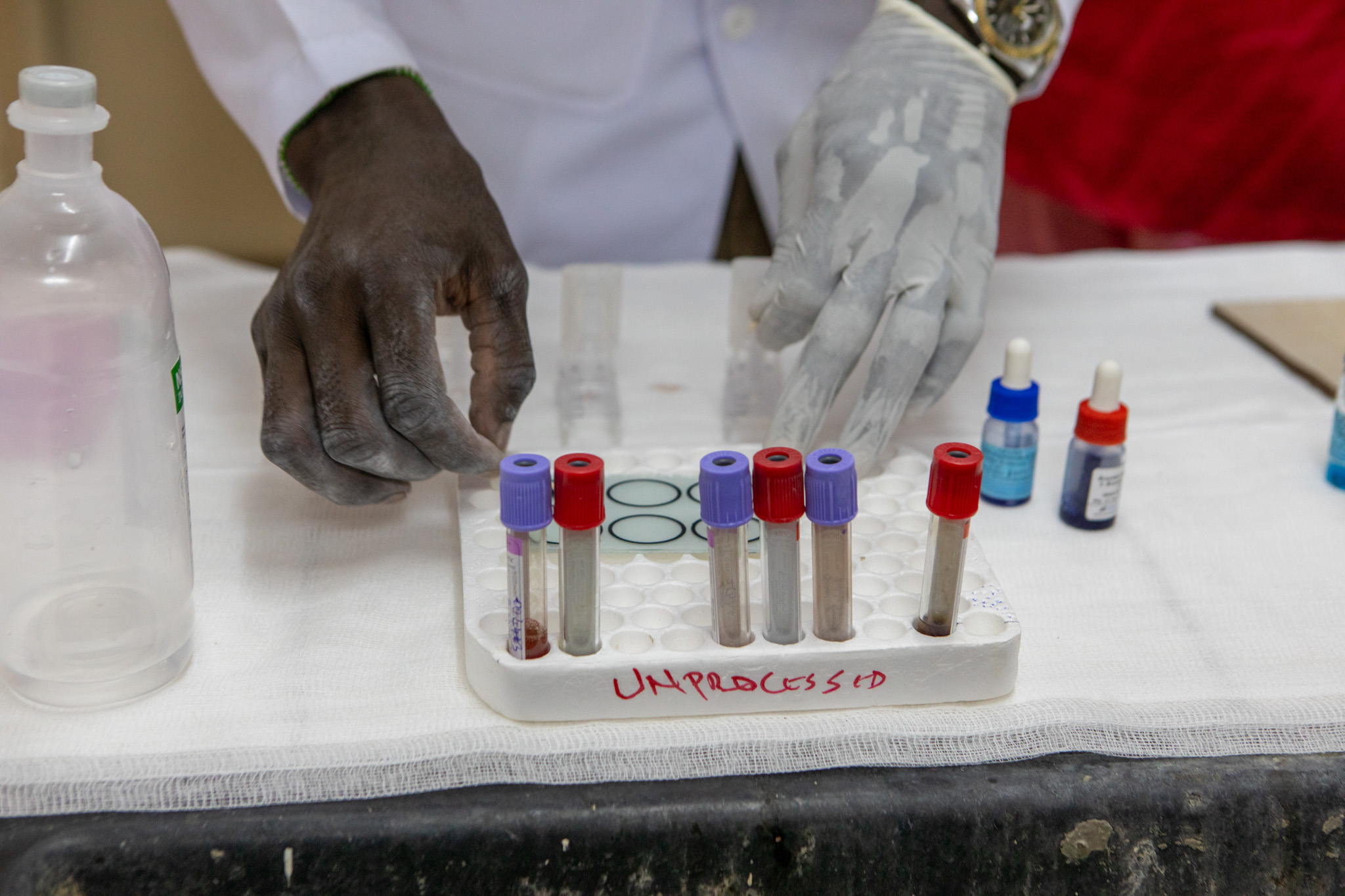
“428 cases this year. 1,000 pints of blood are needed per quarter. Only 120 collected from volunteers, and requires to be sent more than 360 km away for screening!” Alice Nataba, Turkana’s Laboratory Services Coordinator, recites the numbers like a grim chant.
Kenya’s blood donation rate remains low, with less than 10 per 1,000 people donating blood, with the situation in Turkana being more dire, earning the nickname “blood desert” according to an article in The Guardian.

In a nearby ward, seven-year-old Kale Nikimat curls into herself, her belly grotesquely distended, with visible scars on her swollen tummy.
Her uncle brought her here after traditional healers carved these marks into her skin, mistaking her illness for malaria.
Her mother knew nothing about this Kala-azar disease, but admits to her girl playing in sandbanks next to Lake Turkana.
Neighbours called the uncle when she began to fade. Without his intervention, she would already be gone.
Nurse Juliet moves from Kale’s bed, tending to various patients.
“We lost eight from Philip’s village here last month. All from kala-azar. But something strange happened! When they came, they all bled. Some from the nose, others were swollen before we could even start treatment,” she said, her voice heavy.
The current first-line treatment in East Africa is a combination of Sodium Stibogluconate (SSG) with Paromomycin (PM) for 17 days.
It requires two painful injections daily, which can affect the heart, liver, kidneys, and pancreas.
The average cost of treating a patient is Sh30,000 (approximately USD230).
While treatment is often free in endemic areas, access remains a major barrier.
The shortage is lethal. Kala-azar patients need blood before treatment can begin.
But pastoralist beliefs that giving blood weakens the body discourage donation, with some demanding their blood back if it is deemed unfit for transfusion.
Others live too far, in places like Turkana East, where banditry makes travel, even to the hospital, life-threatening.
Clinics lack RK-39 test kits, refrigerators for the blood, ambulances for referrals, basic drugs, and food for the patients.

Some patients flee to Uganda, where outreach programs offer free treatment at Amudat Hospital in Amudat District.
In Namorputh, a nurse spends Sh4,000, a fortune, to hire a vehicle just to transport blood for a patient.
“We had 65 patients in a single day. Our health system was overwhelmed,” James Ekamais, Turkana’s Neglected Tropical Diseases Coordinator, speaks with weary frustration.Most are boys and young children, herders between 5 and 15 years old, bitten by sandflies in the cool of dawn.
Turkana County, the Ministry of Health in Kenya, Amref Health Africa, with financial support from The END Fund, and other partners are intervening but need more help.
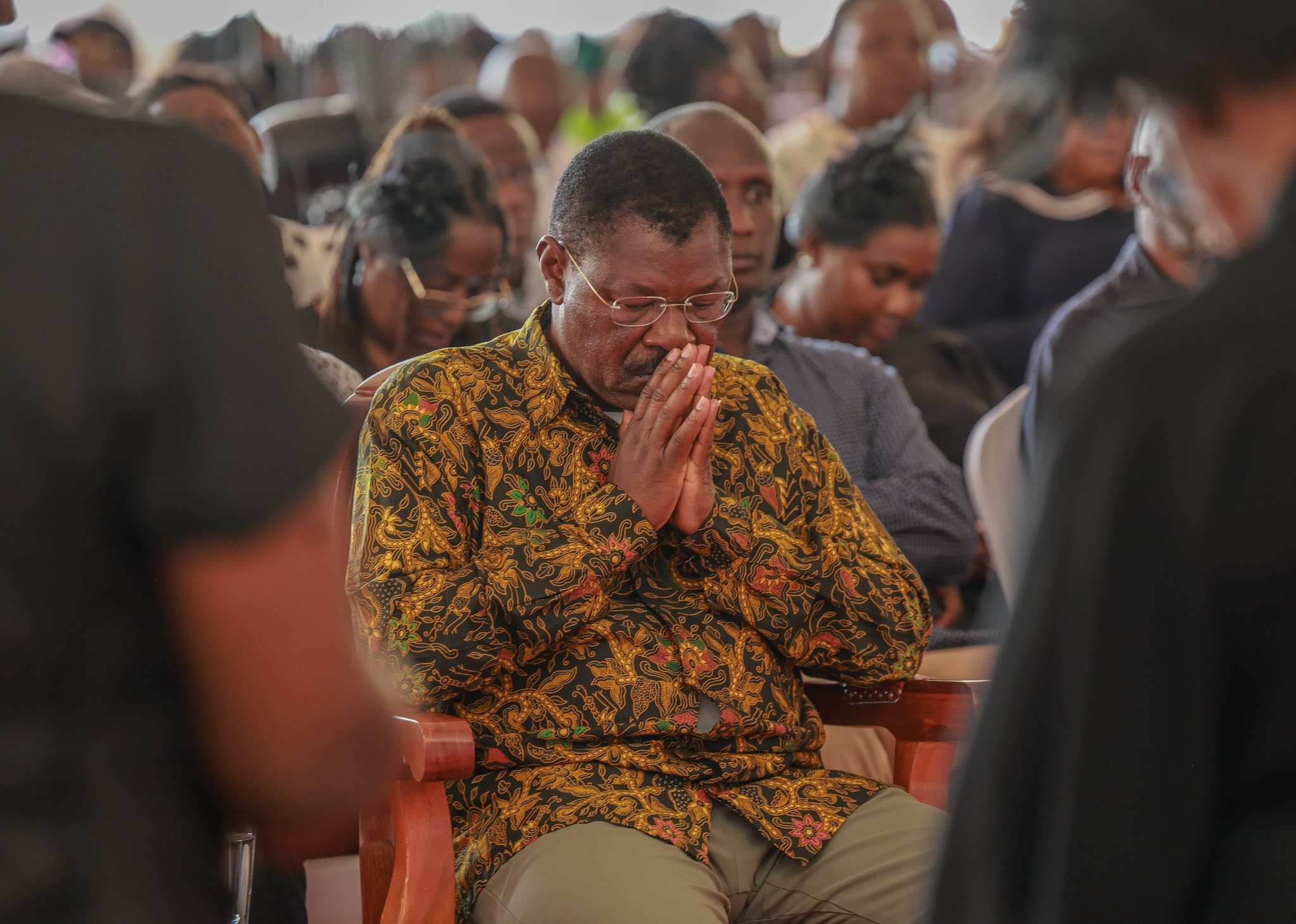
Moses Abraham Kutwah, an NTD Volunteer, is part of this dedicated team conducting active case searches.
They lead mobile clinics through remote villages, screening feverish children and adults with swollen abdomens under acacia trees.
Not even the gunshots too loud during these outreaches in Lokori can stop them.
“We train health workers. But we need more than knowledge. We need a regular supply of test kits, drugs, blood, and nutritious food,” he says.
Amref is supporting national and county strategies to eliminate Kala-azar through the development of a national strategic plan for the elimination of visceral leishmaniasis and revision of the national treatment guidelines.
Other support strategies include vector control, surveillance, community engagement, capacity building of national and county healthcare workers, and active case search.
They help communities understand the disease, its side effects, and the importance of early treatment.
A beneficiary of these outreaches at PAG Lokwatuba in Loima is Nurse Simon Nanok. He has learned to spot Kala-azar the moment a patient walks in.
He knows the signs: prolonged fever, weight loss, enlarged spleen and liver, anemia, and bleeding tendencies.
He pastes educational posters on his clinic walls, a small act of resistance against this deadly disease.
Amana Eregae, a Community Health Promoter, knows and follows up on all her households.
She guides visitors through thorny shrubs to a homestead where an anthill looms, full of sandflies, a silent killer just steps from where children sleep.
At this homestead, two children have recently recovered from Kala-azar thanks to early treatment.
Kenya is among 10 countries globally that account for 90% of global Kala-azar cases, according to the WHO.
Between July 2024 and June 2025, Kenya recorded its highest number of VL cases on record with over 2,200 cases from 12 endemic counties: Turkana, Baringo, Isiolo, Marsabit, Mandera, West Pokot, Kajiado, Tharaka Nithi, Kitui, Garissa, and Wajir with a new recent foci identified in Samburu.
Kala-azar does not discriminate, although it mainly affects school-going children between 5-14 years; younger children and adults too are affected.
In Turkana, over 400 cases have been identified in 2025, where roads are treacherous and designated treatment centres are few, the fight for survival is fought in fragments, one transfusion, one motorbike ride, one fragile breath at a time.

As night falls on Lodwar Hospital, Philip slips into unconsciousness.
A few moments before he dies, blood finally arrives through a donation that was not used on a pregnant mother during a cesarean section, but his body is too swollen to take it in.
His wife clutches his hand, knowing he will never see their family or his goats again. Next door in the children’s ward, seven-year-old Kale can barely eat.
Her eyes are swollen, and her uncle never leaves her side. Her tiny fist clenches the black synthetic mattress cover, not ready to let go.
At the nurses’ desk, Juliet continues with her paperwork and prepares for another long shift. New faces now lie where Philip once slept.
She will learn their names, meet their families, and smile with them, knowing too well that if they are Kala-azar patients who have a delayed encounter seeking the correct treatment, more bleeding and desperation await.
Yet the rest of the world, away from Lodwar moves on, unaware of this killer desert disease.