Kenya's public health system has received a significant boost after the government finally moved to post medical, pharmacy, and dental interns who had awaited placements for months.
The deployment of over 6,484
healthcare interns, including 2,000 medical doctors, brings relief to
overstretched hospitals and offers young professionals the opportunity to gain
much-needed experience.
This bold move has been welcomed by medical graduates, healthcare facilities, and stakeholders as a lifeline for both strained hospitals and hopeful young professionals. It marks a major step in addressing youth unemployment.
Yet beneath the optimism lies a deeper concern: will practicing doctors finally receive their long-overdue arrears? And can the system sustain these postings and payments in the years to come?
The system currently relies on both domestic and foreign donor funds — a framework that can, at times, prove unpredictable.
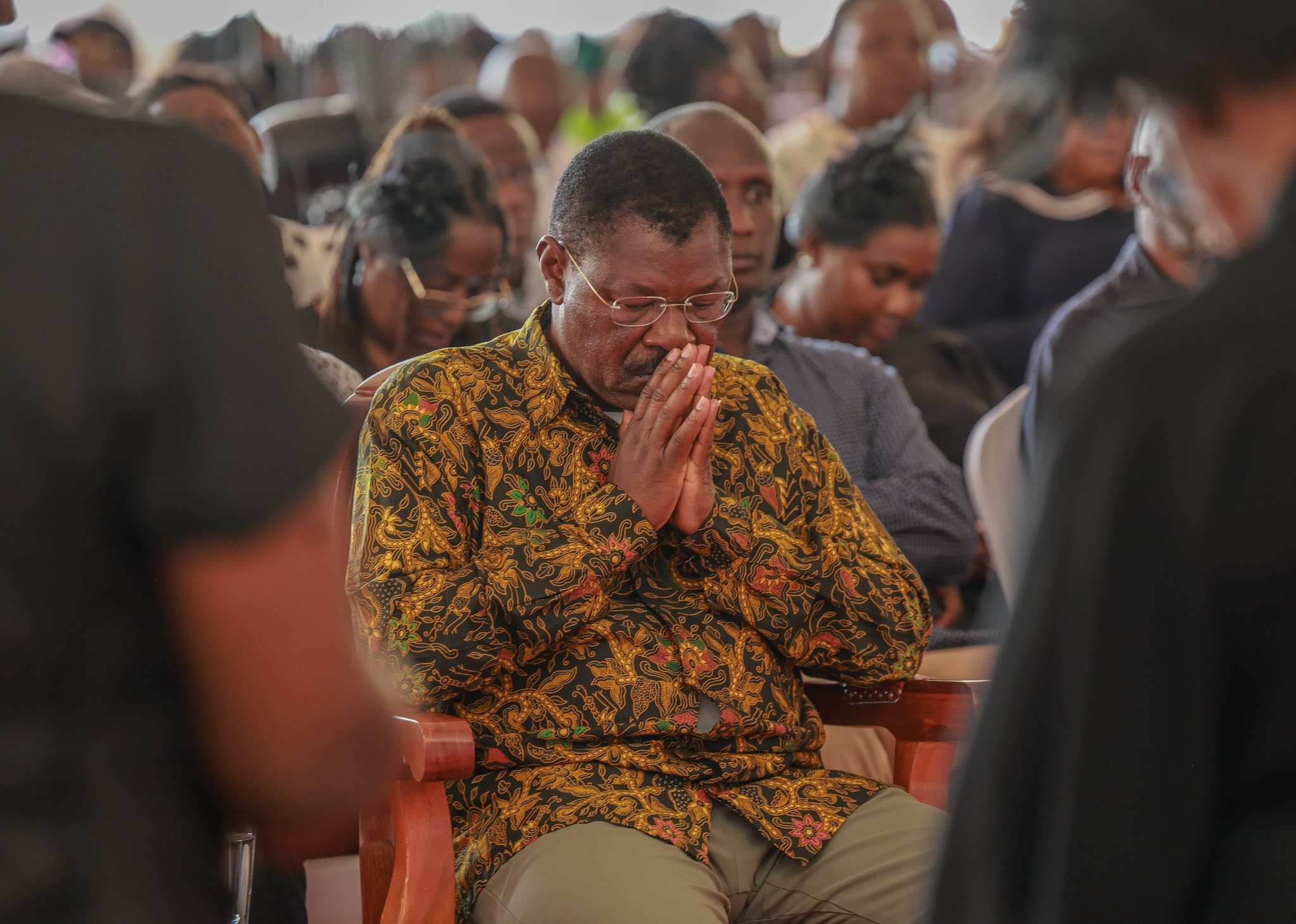
The Ministry of Health announced the posting of interns in July 2025, ending months of uncertainty for graduates. Cabinet Secretary for Health, Aden Duale, flagged off the internship program, describing it as a bold demonstration of the government’s resolve to fulfill its promises to Kenya’s healthcare workforce.
This move marks a pivotal shift — one that not only addresses chronic unemployment among medical graduates but also restores hope to thousands of youth. In addition to doctors, the interns hired include pharmacists, dentists, clinical officers, and nurses — part of a broader push to strengthen universal health coverage. The government allocated KSh 4.5 billion to this initiative.
Hospitals, especially in rural areas, are already reporting relief as interns help ease heavy workloads in maternity wards, emergency units, and general clinics. These freshly trained health workers offer a timely fix to acute staffing gaps, making visible contributions while gaining critical exposure.
Yet even as this milestone is celebrated, anxiety lingers. Data from the Kenya Medical Practitioners, Pharmacists and Dentists Union (KMPDU) shows that many doctors have not received their Collective Bargaining Agreement (CBA) arrears.
Some arrears date back as far as seven years. Kenya continues to face a critical shortage of doctors — fewer than 15 per 100,000 people — far below the World Health Organization’s recommended 44 per 100,000. Meanwhile, physicians on the ground remain overworked, understaffed, and demoralised.
While the government is to be applauded for posting interns, it must also clear arrears for practicing doctors and develop a sustainable plan to prevent future crises.
If Kenya is serious about achieving its universal health coverage goals, the proficiency and well-being of its medical professionals cannot be overlooked. The young interns stepping into public hospitals bring fresh knowledge, but the seasoned practitioners — those who have held the system together through years of staff shortages — are often unpaid or underpaid. This is not simply a wage dispute; it is about valuing professionalism, experience, and expertise.
Interns may fill gaps for now, but frontline doctors — with skills, diagnostic mastery, and institutional memory — remain essential. Unless these issues are addressed, the imbalance risks reversing the gains made through intern deployment.
Sustainability hinges on coordination and funding. Ensuring continuity requires predictable financing and coordination across all levels of government. Adequate treasury allocation and increased health budgets are necessary to support both interns and seasoned doctors without defaulting on promises.
Timely disbursement by the Ministry of Health, in coordination with county governments, is essential to ensure salaries and allowances reach recipients without delay. Accountability and oversight are key to preventing the annual disruptions that undermine morale and service delivery.
Posting interns is undoubtedly a forward step and a meaningful victory in reducing youth unemployment. However, for this gesture to translate into lasting reform, Kenya’s healthcare system must deliver on its commitments to practicing doctors — clearing arrears, ensuring timely pay, and building a robust workforce structure that can withstand financial strain. Without predictable budgets, Kenya risks repeating the annual disruptions that harm doctors' morale and delay patient care.
The government's action to post interns reflects responsiveness and a commitment to healthcare reform. It offers hope to young doctors who had felt forgotten. But for frontline doctors battling daily patient loads, hope must be matched with timely pay. Salaries and allowances are not a privilege; they are an investment in Kenya’s universal health coverage goals.
Conclusion
Posting interns is a step forward. Ensuring doctors are paid on time and building a healthcare workforce system that can withstand future budget pressures is the true test. For the system to truly flourish, the proficiency and dedication of experienced doctors must be honoured, not just in words, but in pay.