 Devolution need not be reversed wholesale, but its architecture demands strategic recalibration.
Devolution need not be reversed wholesale, but its architecture demands strategic recalibration.
While localized governance has improved infrastructural visibility and political responsiveness in some counties, the case of public health paints a far grimmer picture: one of fragmentation, professional attrition, and resurgent disease burdens.
If the central government's health apparatus once resembled a tightly coordinated neural network, devolution has left it with a severed spine. The Erosion of National Cohesion in Disease Control Public health systems thrive on central coordination, uniformity of standards, and the capacity to mount rapid responses to emergent threats.
These are not functions best left to 47 independent entities, each with its own political calculus, fiscal priorities, and institutional maturity. The decentralization of such a system has created regulatory and operational discontinuities—visible in the asynchronous disease surveillance, under-reporting, and siloed responses that have characterized recent outbreaks.
From cholera in Kisumu to measles in Wajir, the return of previously controlled diseases illustrates a profound breakdown in preventive health systems. Capacity Disparities: A Matter of Life and Geography Devolution has also amplified existing inequities in health workforce distribution. Counties with limited fiscal muscle—especially in arid or remote regions—have become human resource deserts, unable to attract or retain public health specialists.
These shortages affect not just clinical care but the core functions of inspection, community health mobilization, epidemiological intelligence, and lab-based diagnostics. This unevenness is not a benign feature of local governance—it is a public health risk multiplier.
The Politicization of Public Health Enforcement One of the most corrosive effects of devolved public health has been the subordination of technical enforcement to political patronage.
Public health officers, mandated to close unsafe premises, regulate sanitation, or disrupt hazardous practices, are routinely undermined by local political actors—often motivated by electoral expediency rather than public safety. Without institutional independence, legal protection, or centralized oversight, enforcement has become arbitrary, timid, or entirely absent.
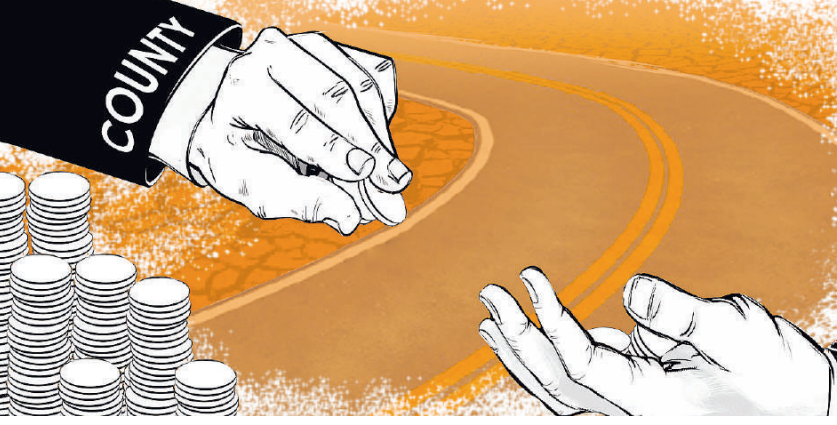
What Should Be Done? Devolution need not be reversed wholesale, but its architecture demands strategic recalibration. A differentiated model—where core public health functions such as surveillance, vaccination, and emergency response remain under strong national stewardship,would preserve coherence and accountability.
Meanwhile, counties can retain operational responsibilities tailored to local context, under a unified legal and technical framework. We must also establish intergovernmental compacts that allow resource pooling, data harmonization, and talent sharing.
A health crisis in Busia should trigger a national response,not bureaucratic hand-wringing about jurisdiction. Finally, public health officers must be insulated from political interference through statutory reforms that guarantee their professional autonomy and provide mechanisms for independent enforcement.
Conclusion: From Aspirations to Accountability Kenya’s devolution framework was built on the laudable aspiration of equity and inclusion. But in the case of public health, it has created a vacuum where coordination once stood. This is not merely a governance failure; it is a bio-political liability. As climate change, urban density, and globalization reshape the epidemiological landscape, we cannot afford a public health system crippled by localism and politics.
The time to reform is now,before the next outbreak reminds us, yet again, that disease does not respect county borders.
Benjamin Kobia Kilemi is a Public Health Specialist and advocate for evidence-based health systems reform.














